Posted By
Chaya Gray
Date
April 24, 2025
Comments
0
LOW BACK PAIN – WHY IT HAPPENS AND HOW IT HEALS
Free Knowledge from Clinical Experience – A Calm, Clear Guide to Healing Your Back
A small note before we begin-
This article is written the same way I talk to my patients in the clinic — slowly, calmly. Low back pain can feel scary, but in most people, it is not a serious spine problem. It is a muscle, posture, and movement problem — and that means it can be corrected.
Many people are told:
“Your disc is damaged.”
“Your spine is weak.”
“You must rest forever.”
But the truth is this:
Your spine is one of the strongest structures in your body.
What usually fails is the support system around it — the muscles.
When muscles become weak, tight, or tired, the spine starts to take stress — and that creates pain.
The good news?
Muscles can be trained, relaxed, and healed at any age.
This guide will take you step by step — just like a physiotherapy treatment plan — from pain to strength to long-term protection.
STEP 1 – UNDERSTAND WHAT IS REALLY CAUSING YOUR BACK PAIN
Most people think back pain means their spine is damaged.
In reality, in more than 80–90% of cases, the spine is fine.
The pain comes from:
- Weak core muscles
- Tight hip and back muscles
- Long sitting or phone use
- Poor posture
- Stress and fatigue
- Sudden bending, lifting, or twisting
When these muscles stop doing their job, the spine takes too much load — and that creates pain.
Think of it like this:
Your spine is a pole.
Your muscles are the ropes holding it steady.
When the ropes become loose, the pole starts to strain.
That strain is what you feel as pain.
This is why scans often show “disc bulge” or “degeneration” even in people who have no pain — the scan shows structure, not muscle support.
The good news:
Muscles can be trained, relaxed, and strengthened at any age — which means your pain can be reversed.
STEP 2 – CALM THE PAIN AND MUSCLE TIGHTNESS
Before we try to strengthen anything, the first job is to calm the irritated muscles and joints.
A painful back cannot exercise properly — it must relax first.
This step usually takes 3–5 days (sometimes a little longer if pain is severe).
What to do
- Heat Therapy
- Apply a warm pack on the lower back
- 15–20 minutes
- 2 times a day
Heat increases blood flow and allows tight muscles to release.
- Comfortable Positions
Use these positions during rest and sleep:
- On your back → place a pillow under your knees
- On your side → place a pillow between your knees
These positions reduce pressure on the spine.
- What to avoid for now
For a few days, avoid:
- Bending forward
- Lifting
- Floor sitting
- Twisting
- Long standing in one place
This gives irritated tissues time to settle.
STEP 1 – UNDERSTAND WHAT IS REALLY CAUSING YOUR BACK PAIN
Now that pain and spasm have started to calm, the next goal is to bring safe movement back into the spine.
A stiff back stays painful.
A gently moving back starts healing.
This step usually begins after 3–5 days of Step 2 or once sharp pain has reduced.
Do these exercises twice daily
They should feel comfortable and relieving, never sharp or forced.
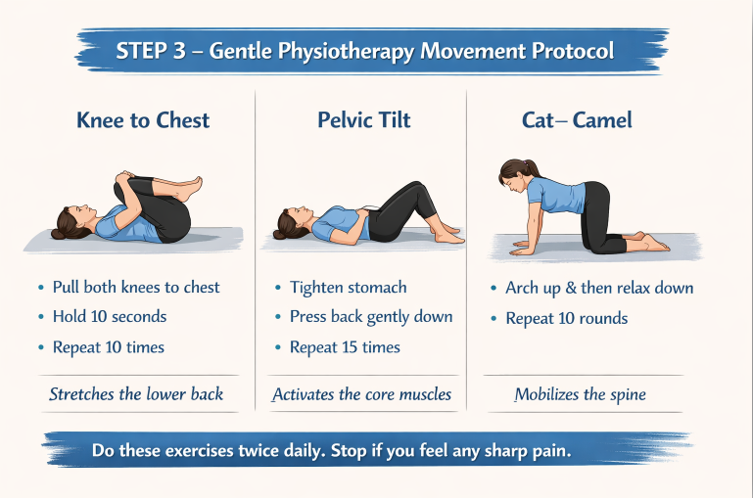
- Knee to Chest – Lie on your back and slowly pull both knees toward your chest, hold for 10 seconds, then relax. Repeat 10 times. This gently stretches tight lower-back muscles and reduces spinal pressure.
- Pelvic Tilt – Lie with knees bent, tighten your stomach and press your lower back gently into the bed, hold for 5 seconds and relax. Repeat 15 times. This reactivates the deep core muscles that protect the spine.
- Cat–Camel – Come onto hands and knees and slowly arch your back up, then relax it down, moving gently with your breath. Do 10 slow rounds. This improves spinal mobility and reduces stiffness.
These exercises should make you feel:
- Looser
- Lighter
- More comfortable
If any movement causes sharp or shooting pain, stop and go back to Step 2 for another day.
STEP 4 – PHYSIOTHERAPY STRENGTHENING PROTOCOL
Once pain and stiffness have reduced and simple movements feel comfortable, the next step is to make the back strong again. This phase is essential because most back pain returns not due to injury, but due to weak support muscles. Strengthening these muscles allows the spine to stay protected during daily activities like bending, lifting, and walking.
This step usually begins after 7–10 days of gentle movement, or when sharp pain has settled and confidence in movement has returned.
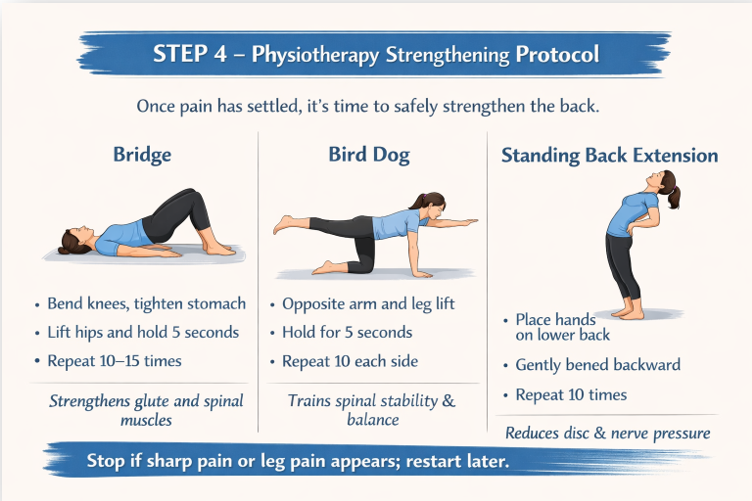
- Bridge – Lie on your back with knees bent, tighten your stomach, lift your hips, and hold for 5 seconds, then lower slowly. Repeat 10–15 times. This strengthens the glute and spinal support muscles.
- Bird Dog – Come onto hands and knees, extend the opposite arm and leg, hold for 5 seconds, then switch sides. Do 10 repetitions each side. This improves spinal stability and balance.
- Standing Back Extension – Stand upright, place your hands on your lower back, gently bend backward, and hold for 3–5 seconds. Repeat 10 times. This reduces disc and nerve pressure.
These exercises should feel controlled and safe. If sharp pain or leg pain appears, return to gentle movement exercises for a couple of days before restarting strengthening.
“When the above feels easy, add these:”
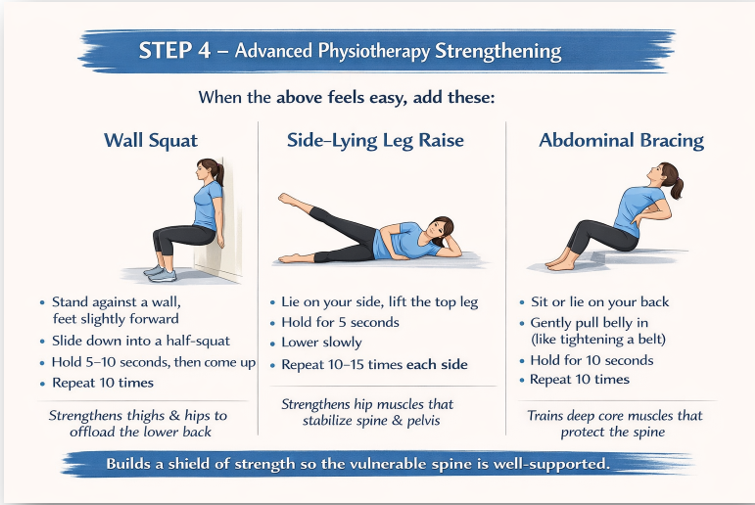
4.Wall Squat
Stand with your back against the wall, feet slightly forward. Slowly slide down into a half-squat, hold for 5–10 seconds, then come up. Repeat 10 times.
This strengthens the thighs and hips, which take load off the lower back.
5.Side-Lying Leg Raise
Lie on your side and lift the top leg straight up, hold for 5 seconds, then lower. Repeat 10–15 times each side.
This strengthens hip muscles that stabilize the pelvis and spine.
6.Abdominal Bracing
Sit or lie comfortably and gently pull your belly in as if tightening a belt. Hold for 10 seconds while breathing normally. Repeat 10 times.
This trains deep core muscles that protect the spine during daily movement.
Why these matter?
Most low-back pain keeps coming back because:
The hips, thighs, and core are weak, not the spine.
By strengthening these areas, the back becomes naturally protected.
STEP 5 – WALKING & DAILY ACTIVITY PROTOCOL
Once pain has reduced and strengthening exercises feel comfortable, the back must learn to work during normal movement. This step reconnects your spine to daily life.
- Walking – Start with 10 minutes of comfortable walking once daily and increase by 5 minutes every few days, aiming for 30–40 minutes. Walking improves blood flow, nourishes spinal discs, and calms the nerves.
- Sitting breaks – Avoid sitting continuously for long periods. Stand up, stretch, or walk for 1–2 minutes every 30–40 minutes. This prevents stiffness and muscle fatigue.
- Safe bending – When picking up objects, bend at the hips and knees instead of the lower back, keeping the object close to your body. This protects the spine from strain.
- Gradual return to work and chores – Resume daily activities slowly. Avoid sudden heavy lifting or twisting for a few weeks, even if pain has reduced.
Regular walking and mindful activity are what turn exercises into long-term recovery.
STEP 6 – DIET, SUPPLEMENTS & NUTRITIONAL SUPPORT FOR BACK HEALING
Exercises rebuild strength, but healing happens faster when muscles and nerves are well-nourished. Food does not replace physiotherapy, but it strongly supports recovery.
Diet to support healing-
- Protein (eggs, fish, lentils, beans, paneer, tofu) helps repair muscles.
- Fruits and vegetables provide antioxidants that reduce inflammation.
- Healthy fats (nuts, seeds, olive oil, coconut oil) support joints and nerves.
- Spices like turmeric and ginger help control inflammation naturally.
- Adequate water intake keeps spinal discs hydrated.
Avoid excess sugar, fried foods, refined flour, and smoking, as they delay healing and increase inflammation.
SUPPLEMENTS-
Supplements can play a supportive role in low back pain recovery by helping reduce inflammation, improve muscle function, and support tissue healing. However, they work best when used alongside physiotherapy, regular movement, and lifestyle correction—not as a replacement for active treatment. In my clinical practice, I often recommend the following supplements as supportive measures to help manage low back pain, depending on the individual’s condition and overall health.
- Magnesium helps relax tight muscles, reduce spasms and stiffness, and can be especially useful for night pain or muscle tension.
- Vitamin D supports muscle strength and bone health, and low levels are commonly associated with frequent pain and delayed recovery.
- Omega-3 fatty acids help reduce inflammation in joints and soft tissues and may support nerve and overall tissue health.
- Curcumin has natural anti-inflammatory properties and may help reduce pain and inflammatory irritation.
- Collagen (with vitamin C) supports ligaments, tendons, and connective tissue, which can be helpful during healing and rehabilitation.
- Glucosamine supports cartilage health and is usually considered only when joint degeneration or arthritis is also present.
Supplements should be taken only under professional guidance, especially if you have medical conditions.
STEP 6 – LONG-TERM PREVENTION & BACK CARE ROUTINE
- Continue exercises – Even after pain is gone, perform your back and core exercises 3–4 times per week. This maintains strength and prevents recurrence.
- Posture awareness – Sit with lower-back support, keep screens at eye level, and avoid slouching or prolonged phone use. Small daily corrections protect the spine.
- Safe lifting habits – Always bend from the hips and knees, keep objects close to the body, and avoid sudden twisting movements.
- Regular walking – Maintain 30–40 minutes of walking most days. This keeps spinal joints mobile and nourishes discs.
- Early response to stiffness – If tightness or mild pain returns, restart gentle movement and heat therapy early instead of waiting for pain to worsen.
Consistency is the key.
A back that is regularly moved, strengthened, and respected stays pain-free for years.
Common Questions About Low Back Pain
Q1. Is low back pain always caused by disc problems?
No. In most people, low back pain is not caused by serious disc damage. It usually comes from muscle weakness, tightness, poor posture, prolonged sitting, or sudden strain. Many people with disc bulges have no pain at all. Pain often reflects muscle and movement issues, not a damaged spine.
Q2. Should I completely rest if I have back pain?
Complete bed rest is usually not recommended. Short periods of rest may help during severe pain, but prolonged rest weakens muscles and delays recovery. Gentle movement, walking, and guided exercises help the back heal faster.
Q3. Is walking good or bad for low back pain?
Walking is generally very good for low back pain once severe pain has settled. It improves blood flow, nourishes spinal discs, relaxes muscles, and calms the nervous system. Start slowly and increase duration gradually.
Q4. Can exercises make my back pain worse?
When done incorrectly or too early, exercises can aggravate pain. However, proper physiotherapy-guided exercises done at the right stage actually reduce pain and prevent recurrence. Exercises should feel comfortable and controlled — never sharp or forced.
Q5. How long does low back pain usually take to heal?
Most uncomplicated low back pain improves significantly within 2–6 weeks with the right approach. Healing depends on muscle strength, posture, daily habits, stress levels, and consistency with exercises.
Q6. Do I need an MRI or X-ray for back pain?
Imaging is not always necessary, especially in the early stages. Scans are usually recommended only if there are red flags such as severe trauma, progressive weakness, numbness, bladder or bowel symptoms, or pain that does not improve over time.
Q7. Can low back pain come back after it heals?
Yes, it can — especially if underlying muscle weakness, poor posture, or sedentary habits are not corrected. This is why long-term exercises, walking, and posture awareness are essential even after pain settles.
Q8. Does stress affect low back pain?
Yes. Stress increases muscle tension and sensitizes pain pathways. Many people notice their back pain worsens during emotional stress, poor sleep, or fatigue. Relaxation, regular movement, and good sleep play an important role in recovery.
Q9. Are supplements necessary for back pain recovery?
Yes, In many patients, supplements can play a supportive and beneficial role by improving muscle relaxation, reducing inflammation, and aiding tissue healing. They are most effective when combined with physiotherapy, regular movement, and healthy lifestyle habits.
Q10. When should I seek professional help?
You should seek professional guidance if pain is severe, persistent, worsening, associated with leg pain or numbness, or if you feel unsure about safe movement and recovery progression.
Final Message-
Low back pain is not a life-long problem.
When pain is calmed, movement is restored, muscles are strengthened, daily activity is corrected, and nutrition is supported, the back heals naturally.
A strong back is not built by rest — it is built by the right movement, at the right time.
If you feel unsure about your symptoms or need individualized guidance beyond general information, you may consider a personal consultation.
Affiliate & Medical Disclaimer
Some links in this article are affiliate links, meaning I may earn a small commission at no extra cost to you. This support allows me to continue creating free, evidence-based health guides, exercises, and educational content. All recommendations are shared based on clinical experience and general wellness principles and are not intended to diagnose or treat medical conditions. Please consult a qualified healthcare professional before starting any supplement or treatment.
About Me
Chaya Gray
Quis autem vel eum iure repreherit qui in ea voluptate velit ess quam nihil molestiae consequatur velab illum denounci pleasure
Recent Blogs

Conveniently deploy accurate …

Conveniently deploy accurate …