Posted By
Chaya Gray
Date
July 31, 2022
Comments
0
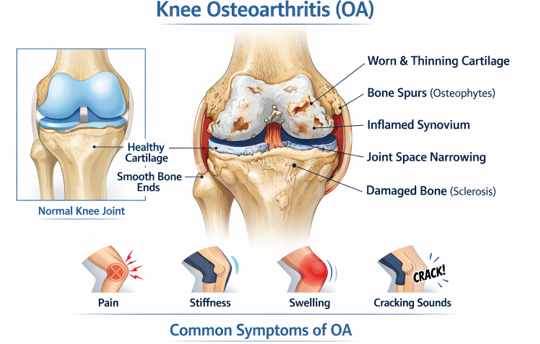
Knee Osteoarthritis (OA)
FREE Knowledge from Clinical Experience – A Story Every Knee Patient Deserves to Hear
A small note before we begin
This article is written the way I speak to my patients in the clinic — calmly, honestly, and without fear. What you read here is free knowledge based on clinical experience and supported by research, explained in simple language.
My Clinical Story with Knee Osteoarthritis Patients
During my 18+ years of clinical practice as a physiotherapist, knee osteoarthritis has been one of the most common problems I see — and not just in elderly patients. I meet people in their 30s and 40s who walk into the clinic worried, confused, and often scared after seeing their X‑ray reports.
Many believe that once cartilage damage starts, pain is unavoidable and surgery is the only future. This is one of the biggest myths I want to clear right away.
In reality, most knee osteoarthritis patients improve significantly when they understand the condition and start the right combination of exercise, diet, and lifestyle changes — at the right time.
What I Have Learned from Treating Knee Osteoarthritis (Clinically)
Over the years, treating hundreds of knee osteoarthritis patients, I have learned one very important thing:
Knee osteoarthritis is not just a “cartilage problem” — it is a movement, muscle, and lifestyle problem.
In my clinical experience, pain often increases not because the knee is “damaged beyond repair,” but because:
- The supporting muscles have weakened
- The joint is not moving correctly
- Daily habits are silently overloading the knee
- Fear and incorrect advice lead to complete rest, which actually worsens the condition
This article is based not on textbook theory alone, but on real patients, real struggles, and real recoveries I have witnessed in my clinic.
What You Will Understand from This Article
- What exactly is knee osteoarthritis beyond what an X-ray shows?
• Why do some people with severe reports have less pain, while others suffer more?
• What are the early warning signs of knee OA that people often ignore?
• Is exercise safe for knee osteoarthritis, or can it worsen the condition?
• Which physiotherapy exercises actually reduce knee pain and improve function?
• How do diet and daily lifestyle habits affect knee inflammation and stiffness?
• Do supplements really help in knee osteoarthritis, and which ones are worth considering?
• When is surgery truly necessary, and when can it be avoided?
STEP 1- Understanding Knee Osteoarthritis (In Simple Words)
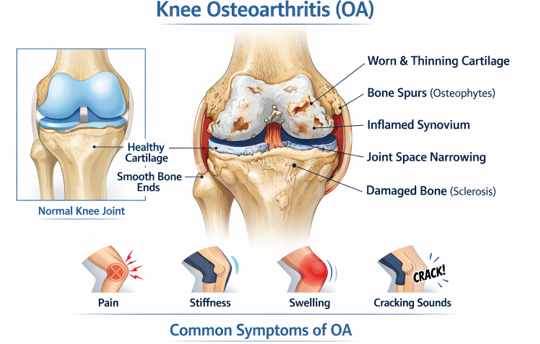
Knee osteoarthritis is not just about “bones rubbing together.” It is a gradual process where the cushioning cartilage inside the knee becomes thinner, the surrounding muscles weaken, and low‑grade inflammation builds up in the joint.
Pain often comes not only from cartilage changes, but also from: – Weak thigh and hip muscles – Reduced joint lubrication due to less movement – Poor movement patterns developed over time
This is why two people with similar X‑ray reports can experience very different levels of pain.
Early Signs People Commonly Ignore
In the clinic, patients often tell me, “It was very mild in the beginning, so I ignored it.” These early signs matter:
- Pain while climbing or coming down stairs
- Stiffness after sitting for a long time
- Discomfort when getting up from the floor or bed
- Mild swelling after excessive walking
- Cracking sounds in the knee without pain initially
Catching OA early makes management much easier.
Grades of Knee OA – What They Really Mean in Daily Life
Patients often panic after reading words like Grade 2 or Grade 3 on reports. Clinically, I always explain this:
- Grade 1–2: Pain is activity‑related and very manageable
- Grade 3: Pain becomes frequent, but function can still improve a lot
- Grade 4: Pain is severe, but even here muscles and lifestyle still matter
An X‑ray does not decide your future — your daily habits do.
What I Commonly Observe in My Patients
Over time, a clear pattern appears in almost every knee OA case:
- Weak quadriceps (front thigh muscles)
- Weak hip and gluteal muscles
- Fear of movement after pain starts
- Weight gain due to reduced activity
- Poor footwear and sitting habits
The good news? All of these can be addressed.
Why Physiotherapy Exercises Matter So Much?
One thing I tell almost every patient is this:
“Your knee is not failing you — your muscles have stopped supporting it.”
STEP 1- Understanding Knee Osteoarthritis (In Simple Words)
One of the most important things knee osteoarthritis patients need to understand is this:
OA is not just a joint problem — it is a movement problem.
As pain starts, people naturally reduce movement. Over time, this leads to muscle weakness, stiffness, reduced joint nutrition, and increased load on already sensitive knee structures. This creates a vicious cycle of –
pain → less movement → more weakness → more pain.
Physiotherapy exercises help break this cycle.
One thing I tell almost every patient is this:
“Your knee is not failing you — your muscles have stopped supporting it.”
The role of exercises in knee OA is to:
- Improve muscle strength around the knee and hip
- Reduce stress on joint surfaces
- Improve joint lubrication through movement
- Increase confidence and reduce fear of activity
- Improve long-term function and independence
Research and clinical experience both show that properly guided exercise is one of the most effective treatments for knee osteoarthritis, often more helpful than medicines alone.
This is why exercise therapy is recommended worldwide as a first-line treatment for knee OA.
Quadriceps Strengthening (Research‑Backed)
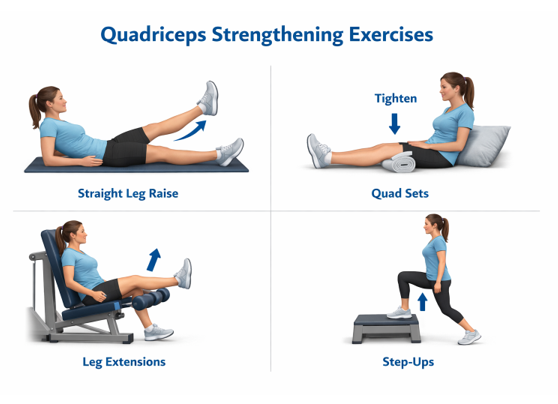
The quadriceps muscle plays a major role in absorbing shock at the knee. Research consistently shows that strengthening the quadriceps reduces knee pain and improves function in people with knee osteoarthritis.
Clinically, patients often report: – Less pain while walking – Better confidence on stairs – Reduced stiffness over time
This is why strengthening exercises are considered a core treatment for knee OA worldwide.
Quadriceps Strengthening Exercises (How to Do Them Safely)
1️⃣ Straight Leg Raise
How to do it:
- Lie on your back on a mat or bed
- Bend one knee, keep the other leg straight
- Tighten the thigh of the straight leg and slowly lift it about 10–12 inches
- Hold for 3–5 seconds, then slowly lower
Repetitions:
8–10 reps × 2–3 sets
Clinical tip:
If pain increases, reduce the height of the lift.
2️⃣ Quad Sets (Very Important for Beginners)
How to do it:
- Sit or lie with legs straight
- Place a rolled towel under the knee
- Tighten the thigh muscle and press the knee down into the towel
- Hold for 5 seconds, then relax
Repetitions:
10–15 reps × 2–3 sets
Clinical tip:
This exercise is safe even during pain or early OA stages.
3️⃣ Leg Extensions (Seated)
How to do it:
- Sit on a chair with feet on the floor
- Slowly straighten one knee until the leg is fully extended
- Hold for 3 seconds
- Slowly lower back down
Repetitions:
8–12 reps × 2 sets
Clinical tip:
Avoid jerky movements; slow control matters more than speed.
4️⃣ Step-Ups
How to do it:
- Stand in front of a low step or stair
- Place one foot on the step
- Push through the heel and step up
- Slowly step back down
Repetitions:
6–10 reps per leg × 2 sets
Clinical tip:
Use a railing or wall for balance if needed.
Important Safety Notes I Tell My Patients
- Mild muscle discomfort is normal
- Sharp pain inside the knee is not
- Breathe normally — do not hold your breath
- Progress gradually, not aggressively
Consistency matters more than intensity.
Does Exercise Worsen OA?
This is a very common fear. Research clearly shows that properly guided exercise does not worsen osteoarthritis. Instead, it improves joint nutrition, muscle support, and long‑term mobility.
Movement is medicine — when done correctly.
STEP 3- Home-Based Pain Relief That Actually Helps
Small daily habits make a big difference:
Home-Based Pain Relief That Actually Helps
Small daily habits, when done correctly, can significantly reduce knee pain and stiffness. These methods are meant to support movement, not replace exercise or physiotherapy.
- Heat Therapy for Stiffness
Heat helps relax muscles, improve blood flow, and reduce morning or rest-related stiffness.
How to use:
Apply a warm hot-water bag or heating pad over the knee.
When:
Best used in the morning or before exercises.
Duration:
10–15 minutes, 1–2 times a day.
Avoid:
Using heat on a visibly swollen or very painful knee.
- Cold Packs for Swelling
Cold therapy helps reduce inflammation and swelling after activity.
How to use:
Wrap an ice pack or cold pack in a cloth and place it over the knee.
When:
After prolonged walking, standing, or if swelling increases.
Duration:
10–12 minutes, once or twice as needed.
Avoid:
Direct ice on skin or using it for too long.
- Temporary Knee Support During Long Walks
A knee cap or support can provide warmth, mild compression, and confidence during activity.
How to use:
Wear during long walks, outdoor activities, or travel.
When:
Only during activity — remove it at rest.
Important:
Knee supports are not a replacement for exercises and should not be worn all day.
- Activity Pacing Instead of Complete Rest
Doing too much at once or avoiding movement completely both worsen knee OA.
How to practice:
Break activities into smaller sessions with rest in between.
Example:
Instead of one long walk, do two shorter walks.
Goal:
Stay active without triggering flare-ups.
Pain relief strategies work best when combined with regular exercises and healthy daily habits. The aim is to keep the knee comfortable enough to stay moving.
STEP 4- Diet for Knee Osteoarthritis – An Often-Missed Piece
Many patients focus only on medicines and forget that osteoarthritis has an inflammatory component.
Research suggests that chronic low‑grade inflammation can influence pain and stiffness. This is where diet plays a supportive role.
Helpful dietary focus:
Helpful Dietary Focus for Knee Osteoarthritis
Diet supports muscle strength and helps reduce low-grade inflammation that can influence knee pain and stiffness. The goal is consistency, not strict dieting.
- Adequate Protein for Muscle Strength
Protein helps maintain and rebuild the muscles that support the knee joint.
- Eggs
- Milk, yogurt, cheese (where tolerated)
- Legumes: lentils, chickpeas, beans
- Soy products: tofu, tempeh
- Nuts and seeds
- Fish and lean meats (where applicable)
- Fruits and Vegetables Rich in Antioxidants
Antioxidants help reduce inflammation and support joint health.
- Leafy greens (spinach, kale, lettuce)
- Berries (strawberries, blueberries, raspberries)
- Citrus fruits (oranges, lemons, grapefruit)
- Apples, pears
- Tomatoes, bell peppers
- Broccoli, cauliflower, cabbage
Aim for variety and color on the plate.
- Omega-3 Sources (Anti-Inflammatory Fats)
Omega-3 fatty acids are known to support joint health.
Common sources:
- Fatty fish (salmon, sardines, mackerel)
- Flaxseeds and chia seeds
- Walnuts
- Omega-3 fortified foods (where available)
Plant-based sources are suitable for vegetarians.
- Good Hydration
Adequate hydration helps maintain joint lubrication and muscle function.
Simple guidelines:
- Water should be the primary drink
- Herbal teas and clear soups can contribute
- Limit sugary drinks and excess caffeine
A good general rule is regular small sips throughout the day.
📌 Key reminder for patients:
Diet alone will not cure knee osteoarthritis, but the right food choices can support pain control, muscle strength, and recovery when combined with exercise and lifestyle care.
5. Foods that may worsen symptoms:
- Excess refined sugar
- Highly processed foods
- Frequent fried and packaged foods
Diet won’t cure OA — but it can make pain easier to manage.
Lifestyle Changes That Slow Knee Damage
In clinical practice, these changes often matter more than medicines:
- Maintaining a healthy body weight (reduces joint load)
- Avoiding prolonged sitting
- Using stairs mindfully
- Wearing supportive footwear
- Supporting knees during sleep
- Managing stress (inflammation increases with stress)
Consistency matters more than perfection.
STEP 5- Supplements – Honest, Simple Guidance
Patients often ask about supplements. Here’s the honest view. From my clinical experience, supplements can be helpful for some knee osteoarthritis patients, especially when pain, stiffness, or inflammation limits their ability to exercise comfortably. When chosen correctly, supplements may support pain reduction, improve tolerance to movement, and assist recovery — but they are never a standalone treatment.
The real benefit of supplements is that they can make it easier for patients to stay active, perform exercises with less discomfort, and maintain consistency, which is where true improvement happens. Results vary from person to person, and benefits are usually gradual rather than immediate.
This is why I consider supplements as supportive tools, not cures — useful when combined with physiotherapy, movement, diet, and lifestyle care.
Based on clinical use and available evidence, the following supplements may support knee osteoarthritis management:
- Curcumin (from Turmeric)
Curcumin is the active compound in turmeric. Research shows it has anti-inflammatory properties and may help reduce knee pain and stiffness when used regularly. It works best alongside exercise, not alone.
Commonly used forms: standardized curcumin with black pepper extract (piperine).
- Boswellia
Boswellia is a herbal extract known to block inflammatory pathways. Studies suggest it may improve pain and walking ability in knee OA patients.
Commonly used forms: Boswellia serrata extracts.
- Collagen
Collagen (supportive):
Collagen provides key building blocks for connective tissues such as cartilage, tendons, and ligaments. In some individuals with knee osteoarthritis, collagen supplementation may help reduce pain and improve joint function, particularly when combined with adequate protein intake and exercise. Some studies indicate it may support joint comfort, especially when combined with strengthening exercises.
Commonly used forms: hydrolyzed collagen powders or capsules.
- Vitamin D
Vitamin D is important for muscle and bone health. Deficiency has been linked with increased knee pain and weakness. Supplementation may help if levels are low.
- Omega-3 Fatty Acids
Omega-3 fatty acids are known for their anti-inflammatory effects and may help reduce joint inflammation and stiffness in knee osteoarthritis. Clinically, some patients report less morning stiffness and better movement comfort when omega-3 intake is adequate.
Omega-3s support joint health by helping balance inflammatory processes in the body, especially when dietary intake is low.
Common sources:
- Fish oil (EPA & DHA)
- Algal oil (plant-based option)
Supplements support recovery — they do not replace movement, lifestyle care and medical treatment.
STEP 6- Supportive Products Commonly Used in Knee OA (Optional Aids)
These are supportive tools, not permanent solutions. I usually recommend them only when they help patients stay active and comfortable.
Knee Cap / Knee Support
Used short-term to provide warmth and confidence during walking or long standing. It should not replace muscle strengthening.
Resistance Bands
Very useful for home-based strengthening of quadriceps, hamstrings, and hip muscles. Suitable for beginners and long-term use.
Hot & Cold Packs
Heat helps reduce stiffness, while cold packs help control swelling after activity.
Orthopedic Knee or Leg Pillow
Helps maintain knee alignment during sleep, especially for side sleepers with knee pain.
Do’s & Don’ts I Tell My Patients
Do: – Stay active – Strengthen muscles regularly – Respect pain signals
Don’t: – Completely stop movement – Depend only on painkillers – Panic after reading reports
When Is Surgery Actually Needed?
Most knee OA cases do not need surgery, especially in early and moderate stages. Surgery is considered when pain and functional limitation severely affect daily life despite proper conservative care.
Even after surgery, exercise and lifestyle management remain essential.
A Final Reassuring Note
Knee osteoarthritis is not the end of movement or independence. With the right understanding, exercises, diet, and lifestyle choices, many people live active, comfortable lives without surgery.
This article shares the same free knowledge I give my patients — so you can take informed steps toward better knee health.
Frequently Asked Questions (FAQs)
Can knee osteoarthritis be reversed?
Knee osteoarthritis cannot be completely reversed, but symptoms can be significantly reduced and function can improve with proper exercise, diet, and lifestyle changes.
Is walking good or bad for knee OA?
Walking is generally beneficial when done at a comfortable pace and on even surfaces. Excessive or painful walking should be avoided.
Should I stop exercising if my knee hurts?
No. Complete rest often worsens stiffness and weakness. Exercises should be modified, not stopped.
Do supplements really work for knee OA?
Supplements may help reduce pain and stiffness for some people, but they work best when combined with exercise and lifestyle care.
When should I consider surgery?
Surgery is usually considered only when pain and functional limitation severely affect daily life despite proper conservative management.
Need Personalized Guidance?
If you feel unsure about your symptoms or need individualized guidance beyond general information, you may consider a personal consultation.
Medical & Affiliate Disclosure
Some links in this article are affiliate links, meaning I may earn a small commission at no extra cost to you. This support allows me to continue creating free, evidence-based health guides, exercises, and educational content. All recommendations are shared based on clinical experience and general wellness principles and are not intended to diagnose or treat medical conditions. Please consult a qualified healthcare professional before starting any supplement or treatment.
About Me
Chaya Gray
Quis autem vel eum iure repreherit qui in ea voluptate velit ess quam nihil molestiae consequatur velab illum denounci pleasure
Recent Blogs

Conveniently deploy accurate …

Conveniently deploy accurate …