Posted By
Chaya Gray
Date
July 31, 2025
Comments
0
Cervicogenic Headache: Why Fixing Your Neck Can Stop Head Pain
Introduction
Many people suffer from headaches for years without realizing that the problem is not in the head at all.
In cervicogenic headache, the pain originates from the neck and is felt in the head.
This type of headache is commonly seen in people who:
- Sit for long hours
- Use mobile phones or laptops extensively
- Have poor posture
- Experience neck stiffness or shoulder tightness
Because the neck and head share nerve connections, irritation in the cervical spine can refer pain to the head, temples, forehead, or behind the eyes.
The good news is that cervicogenic headache is highly treatable with the right physiotherapy approach. Medicines may give temporary relief, but correcting neck movement, posture, and muscle support addresses the root cause.
This guide will explain cervicogenic headache step by step, exactly the way it is managed in physiotherapy practice.
STEP 1 – UNDERSTANDING CERVICOGENIC HEADACHE
STEP 1 – Understanding Cervicogenic Headache (From Clinical Experience)
In my clinical experience, many patients come to me complaining of long-standing headaches. They often say they have taken painkillers for years, changed pillows, and even done eye or sinus tests — yet the headache keeps returning.
When I examine them, I usually find that the problem is not in the head at all. The source of pain is the neck.
Cervicogenic headache happens when stiffness, tight muscles, or restricted joints in the upper neck irritate nerves that are connected to the head. Because these nerves share pathways, the pain is felt in the head even though it starts in the neck.
Most patients with cervicogenic headache have:
- Neck stiffness or discomfort
- Tight muscles at the base of the skull
- Poor posture, especially forward head posture
- Pain that is worse with prolonged sitting, phone use, or certain neck movements
The headache is often one-sided and may spread from the neck to the back of the head, temples, or behind the eye. Many patients notice that turning the neck or holding the head in one position for too long increases the pain.
Once patients understand that the neck is the source, the fear reduces. And when i start treating the neck properly, the headache gradually settles.
This is why cervicogenic headache responds very well to physiotherapy — because we treat the cause, not just the symptom.
STEP 2 – WHY CERVICOGENIC HEADACHE HAPPENS?
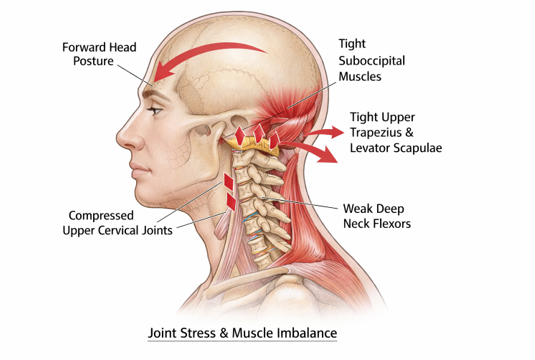
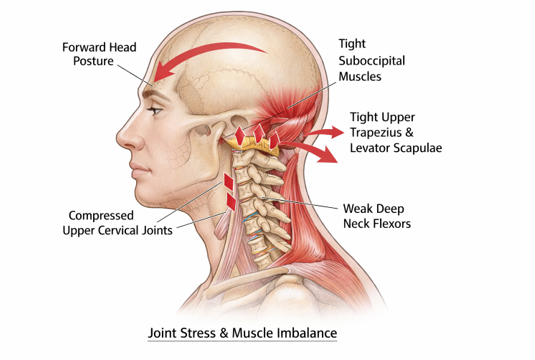
Cervicogenic headache occurs due to dysfunction in the cervical spine, especially the upper neck region (C1–C3). These upper cervical segments have a close neurological connection with the head, which is why problems in the neck can be perceived as head pain.
From a physiotherapy perspective, the most common mechanisms include:
- Upper Cervical Joint Dysfunction
Restricted or irritated joints in the upper cervical spine alter normal movement and stimulate pain-sensitive structures. This joint irritation can refer pain to the back of the head, temples, or behind the eyes.
- Muscle Tightness and Imbalance
Tightness in the suboccipital muscles, upper trapezius, and levator scapulae, combined with weakness of the deep neck flexors, reduces cervical stability. This imbalance increases mechanical stress on the neck and contributes to headache development.
- Poor Posture
Forward head posture, commonly seen with prolonged sitting and mobile or laptop use, significantly increases load on the upper cervical spine. Over time, this sustained stress leads to joint compression and muscle overactivity.
- Sustained or Repetitive Neck Positions
Holding the neck in one position for long durations—such as during desk work, driving, or screen use—can overload cervical structures and trigger referred head pain.
- Previous Neck Strain or Minor Injury
Even a past minor neck strain, repetitive microtrauma, or unresolved stiffness can predispose an individual to cervicogenic headache later.
Because these changes develop gradually, patients often fail to associate their headache with a neck problem. Addressing these mechanical and postural factors is essential for long-term relief rather than temporary symptom control.
Step 3 – How Cervicogenic Headache Feels (Key Symptoms & Patterns)
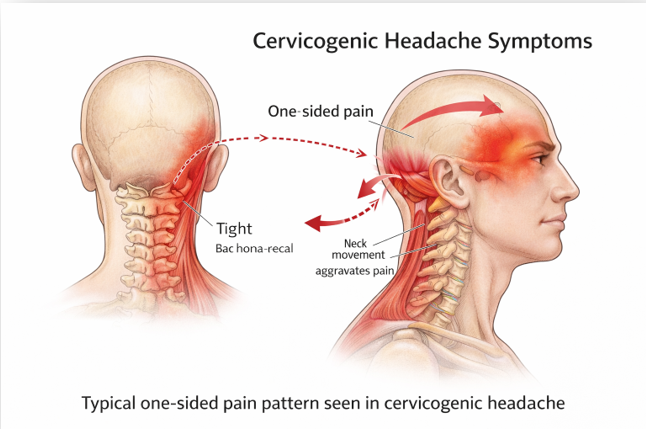
Cervicogenic headache has a characteristic presentation because the pain originates from the neck and is referred to the head. Understanding this pattern helps differentiate it from other common headaches.
Common Symptoms-
Patients with cervicogenic headache typically experience:
- Headache that starts in the neck and spreads to the head
- Pain that is usually one-sided
- Discomfort felt in the back of the head, temple, forehead, or behind one eye
- Neck stiffness or a feeling of heaviness in the neck
- Reduced or painful neck movement, especially rotation or extension
Aggravating Factors
The headache often worsens with:
- Prolonged sitting or desk work
- Mobile phone or laptop use
- Driving or sustained head positions
- Certain neck movements or awkward postures
Associated Findings
Many patients also report:
- Tenderness at the base of the skull
- Tightness in the upper neck and shoulder muscles
- Temporary relief when the neck is supported or rested
How It Differs from Other Headaches
Unlike migraine, cervicogenic headache is not primarily associated with nausea, vomiting, visual aura, or strong light sensitivity. The pain is mechanical in nature and closely linked to neck posture and movement rather than internal neurological triggers.
Recognizing this symptom pattern is crucial, because when the underlying neck dysfunction is treated, the headache often reduces significantly or resolves completely.
STEP 4 – PHYSIOTHERAPY ASSESSMENT (WHAT I EXAMINE CLINICALLY)
When a patient presents with suspected cervicogenic headache, I assess whether the neck is the source of pain.
I evaluate:
- History of headache, including pain pattern, aggravating activities, and posture-related symptoms
- Posture, especially forward head posture and upper body alignment
- Cervical range of motion, noting restriction or pain with neck movements
- Neck muscles and joints, particularly the upper cervical region, to check for tenderness or symptom reproduction
If neck movement, posture, or palpation reproduces the headache, it strongly indicates a cervicogenic origin. This assessment helps guide an effective physiotherapy treatment plan.
STEP 5 – EXERCISES & POSTURE CORRECTION
These exercises aim to improve neck mobility, correct posture, and strengthen supportive neck muscles. They should be performed gently and within a pain-free range.
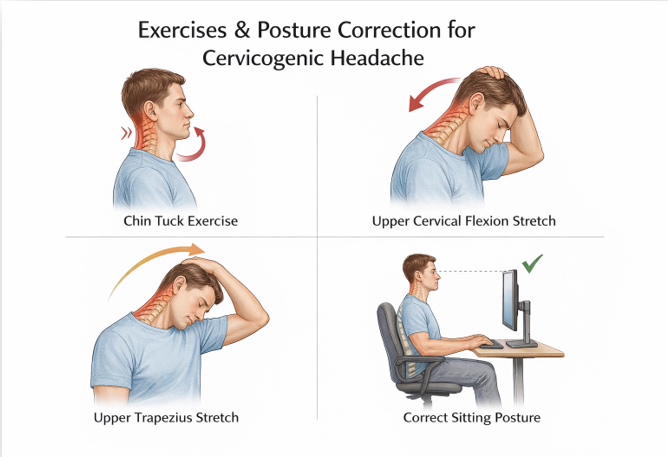
The above exercises form the foundation of cervicogenic headache management. Depending on individual findings, a physiotherapist may add further neck, shoulder, or upper back exercises to optimize recovery.
- Chin Tuck Exercise
How to do it:
Sit or lie comfortably. Gently draw your chin backward as if making a double chin, keeping your eyes level and shoulders relaxed. Hold for 5 seconds, then relax.
Repetitions:
8–10 repetitions, 2–3 times daily
Purpose:
Activates deep neck flexor muscles and corrects forward head posture.
- Upper Cervical Flexion Stretch
How to do it:
Sit upright and gently nod your head forward. Place one hand on the back of your head to apply light pressure until you feel a stretch at the base of the skull.
Hold:
10–15 seconds × 3 repetitions
Purpose:
Relieves tight suboccipital muscles commonly associated with cervicogenic headache.
- Upper Trapezius Stretch
How to do it:
Sit upright and tilt your head to one side. Use the same-side hand to gently increase the stretch while keeping the opposite shoulder relaxed.
Hold:
15 seconds × 3 repetitions on each side
Purpose:
Reduces neck and shoulder muscle tension.
- Posture Correction During Sitting
Key points:
- Screen at eye level
- Ears aligned over shoulders
- Back supported
- Take breaks every 30–40 minutes
Purpose:
Minimizes sustained cervical strain during daily activities.
⚠️ Exercise Precautions
- Perform exercises pain-free
- Stop if headache intensity increases
- Consult a physiotherapist for progression or persistent symptoms
STEP 6 – HOME CARE & DAILY HABITS FOR CERVICOGENIC HEADACHE
Along with exercises, simple daily habits play a major role in preventing recurrence of cervicogenic headache.
- Posture Awareness Throughout the Day
- Keep your head aligned over your shoulders
- Avoid prolonged forward head posture
- Take short posture breaks every 30–40 minutes
- Sleep Position & Pillow Support
- Use a pillow that supports the natural curve of the neck
- Avoid very high or very flat pillows
- Sleeping on the back or side is generally preferred
- Screen & Mobile Use
- Hold mobile phones at eye level
- Adjust laptop or monitor height to avoid neck bending
- Avoid prolonged screen use without breaks
- Heat Application
- Applying a warm pack to the neck for 10–15 minutes can help relax tight muscles and reduce stiffness
- Activity Modification
- Avoid sudden or jerky neck movements
- Gradually return to activities rather than pushing through pain
⚠️ Important Reminder-
Home care supports recovery, but persistent or worsening headaches should always be evaluated by a physiotherapist or healthcare professional
STEP 7- DIET, SUPPLEMENTS & SUPPORTIVE THERAPIES
Cervicogenic headache is primarily treated by correcting neck mechanics through physiotherapy. However, nutrition and supportive therapies play an important role in improving muscle health, reducing fatigue, and supporting recovery, especially when headaches are recurrent or long-standing.
Dietary Support
A balanced diet helps maintain muscle function and postural endurance, which are essential for neck stability.
- Adequate hydration helps prevent muscle stiffness and fatigue
- Protein-rich foods support neck and shoulder muscles
- Eggs, milk, curd, yogurt
- Lentils, beans, chickpeas
- Nuts and seeds
- Anti-inflammatory foods may help reduce chronic tissue irritation
- Fruits and vegetables
- Turmeric, ginger (in moderation)
- Healthy fats such as nuts and olive oil
Skipping meals, excessive caffeine, and highly processed foods may worsen muscle fatigue and should be limited.
Supplements (Supportive)
Supplements can be a useful part of the overall management plan for cervicogenic headache. When chosen appropriately, they help support muscle relaxation, nerve function, and recovery, especially in individuals with increased muscle tension, fatigue, or nutritional gaps. Commonly used supportive supplements include:
- Magnesium – Magnesium plays an important role in muscle relaxation, nerve conduction, and neuromuscular control. In individuals with neck stiffness or postural muscle overactivity, low or borderline magnesium levels may contribute to muscle tightness, fatigue, and increased pain sensitivity.
- Vitamin D – if deficiency is present
- Vitamin B12 – especially in patients with fatigue or nerve-related symptoms
- Omega-3 fatty acids – for general musculoskeletal support
These supplements do not treat the cause of cervicogenic headache but may support physiotherapy outcomes.
Ayurvedic & Traditional Support (Adjunctive Care)
Some patients also benefit from traditional therapies as adjuncts to physiotherapy:
- Nasyam therapy –
Applying 2–3 drops of medicated oil in each nostril may help reduce dryness, stiffness, and heaviness in the head–neck region. It is traditionally used to support comfort in the neck and head area and may be helpful for some individuals with neck-related headaches. - Nasyam is usually done once or twice daily, preferably in the morning, using oils such as Anu taila or plain sesame oil, based on individual tolerance. It should be avoided during active infection, cold, sinus congestion, or immediately after meals.
- Ashwagandha –
May help reduce stress-related muscle tension and improve overall endurance. - Brahmi –
Traditionally used to support mental calmness and reduce stress-related aggravation of symptoms.
These therapies are supportive in nature and should not replace physiotherapy or medical evaluation.
Frequently Asked Questions (FAQs)
- Is cervicogenic headache serious?
Cervicogenic headache is not usually dangerous, but it can significantly affect daily life if left untreated. Because it originates from the neck, proper assessment and treatment help prevent recurrence.
- Can cervicogenic headache be cured permanently?
In many cases, cervicogenic headache improves significantly with physiotherapy, posture correction, and exercises. Long-term relief depends on addressing the underlying neck dysfunction and maintaining good habits.
- How is cervicogenic headache different from migraine?
Cervicogenic headache starts from the neck and is closely related to neck movement and posture. Migraine is usually associated with nausea, light sensitivity, or visual symptoms, which are not typical features of cervicogenic headache.
- How long does physiotherapy take to show results?
Some patients feel improvement within a few sessions, while others may take a few weeks. Consistency with exercises and posture correction plays a major role in recovery.
- Are exercises safe to do at home?
Yes, when performed correctly and within a pain-free range. Exercises should not worsen headache symptoms. If pain increases, professional guidance is recommended.
- Can diet or supplements alone treat cervicogenic headache?
No. Diet and supplements support recovery but do not treat the root cause. Physiotherapy remains the primary treatment approach.
Conclusion
Cervicogenic headache is a neck-related headache that often goes unrecognized for years. Because the pain is felt in the head, many people focus only on medications, while the true source—the cervical spine—remains untreated.
Physiotherapy plays a central role in managing cervicogenic headache by:
- Identifying neck dysfunction
- Correcting posture and movement patterns
- Improving muscle balance and joint mobility
Exercises, posture correction, home care habits, and supportive measures such as proper nutrition and selected supplements can significantly enhance recovery when used appropriately. With the right approach, most individuals experience meaningful and long-lasting relief.
Early recognition and targeted treatment not only reduce headache frequency but also prevent recurrence.
Need Personalized Guidance?
If you feel unsure about your symptoms or need individualized guidance beyond general information, you may consider a personal consultation.
Medical & Affiliate Disclosure
Some links in this article are affiliate links, meaning I may earn a small commission at no extra cost to you. This support allows me to continue creating free, evidence-based health guides, exercises, and educational content. All recommendations are shared based on clinical experience and general wellness principles and are not intended to diagnose or treat medical conditions. Please consult a qualified healthcare professional before starting any supplement or treatment.
About Me
Chaya Gray
Quis autem vel eum iure repreherit qui in ea voluptate velit ess quam nihil molestiae consequatur velab illum denounci pleasure
Recent Blogs

Conveniently deploy accurate …

Conveniently deploy accurate …