Posted By
Chaya Gray
Date
October 11, 2025
Comments
0
TRIGEMINAL NEURALGIA
FREE KNOWLEDGE FROM CLINICAL EXPERIENCE – UNDERSTANDING FACIAL PAIN AND HOW TO MANAGE IT
If facial nerve pain has taken over your daily life, you are not alone — and it does not have to stay this way!
A small note before we begin-
This article is written the way I speak to my patients who come to the clinic with facial nerve pain — calmly and patiently. Trigeminal neuralgia can feel overwhelming at first, but with the right understanding and proper care, many people learn to manage it well and regain confidence in daily life.
What you read here is Free Knowledge based on my clinical experience, explained in simple language, and supported by medical understanding. In this guide, I explain why this pain occurs, what commonly makes it worse, and how it can be approached step by step.
I also share the treatment framework I commonly use with patients, including lifestyle guidance, gentle physiotherapy strategies, and supportive supplements used appropriately. These are not quick fixes, but part of a structured, individualized approach focused on long-term comfort and safety.
My aim is not to create fear — but to replace confusion with clarity, and pain with informed choices.
MY CLINICAL EXPERIENCE WITH TRIGEMINAL NEURALGIA PATIENTS
In my clinical practice, many patients with trigeminal neuralgia come not only in pain, but also mentally exhausted and fearful of triggering symptoms during simple daily activities such as eating, talking, or washing the face.
Over time, I have observed that pain is influenced not only by the nerve itself, but also by neck posture, muscle tension, stress levels, and fear of movement. When patients begin restricting normal activities, this often increases tension and discomfort rather than reducing pain.
While physiotherapy does not directly treat the nerve pathology, gentle techniques used in coordination with medical care can help reduce triggers, calm the nervous system, and improve daily comfort. Improvement is usually gradual, but many patients experience fewer flare-ups and a better quality of life with the right approach.
STEP 1 – UNDERSTANDING TRIGEMINAL NEURALGIA-
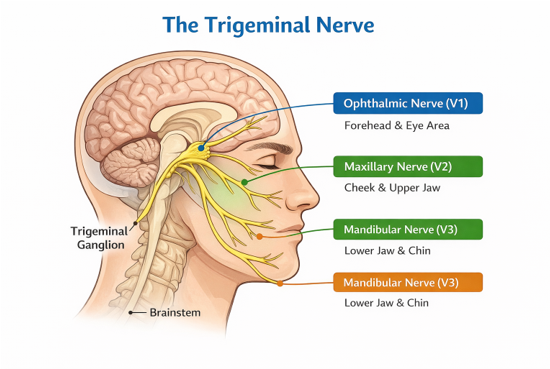
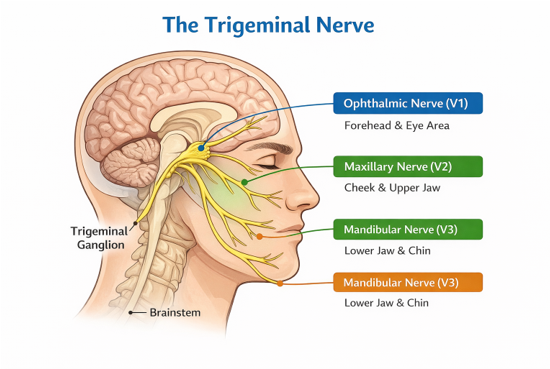
The trigeminal nerve supplies sensation to the face, including the forehead, cheek, jaw, teeth, and gums. Trigeminal neuralgia occurs when this nerve becomes overly sensitive or irritated.
Pain is commonly described as sudden, sharp, electric, or stabbing. Episodes may last seconds or longer and can be triggered by light touch, activities such as washing the face or brushing teeth, talking, or exposure to cold air.
It is important to understand that trigeminal neuralgia is not a sign of facial damage or weakness. Many scans appear normal, and the pain does not mean the facial muscles are failing.
Pain intensity varies widely between individuals. Stress, fatigue, poor neck posture, and anxiety can heighten nervous system sensitivity, making episodes feel more frequent or intense.
COMMON TRIGGERS IN TRIGEMINAL NEURALGIA
Many patients with trigeminal neuralgia notice that pain episodes are triggered by simple, everyday actions. While triggers vary between individuals, some common patterns are often seen in clinical practice.
Commonly reported triggers include:
- Washing or touching the face
- Brushing teeth
- Chewing or talking
- Cold air or wind on the face
- Stress, anxiety, or fatigue
It is important to understand that these triggers do not mean the face is weak or damaged. They reflect heightened nerve sensitivity, where normal sensations are perceived as painful.
STEP 2 – HOW I GUIDE PATIENTS TO DEAL WITH TRIGGERS
One of the first things I explain to patients is that completely avoiding all triggers can increase fear and sensitivity over time.
Instead, the focus is on:
- Identifying personal triggers calmly
- Reducing sudden or aggressive exposure (such as very cold air)
- Maintaining gentle daily activities within comfort
- Managing stress, posture, and muscle tension, which strongly influence nerve sensitivity
Small adjustments — such as using lukewarm water for face washing, protecting the face from cold wind, and maintaining relaxed neck posture — often help reduce flare-ups. With proper medical care and gentle physiotherapy support, many patients gradually regain confidence in daily activities and experience fewer pain episodes.
WHAT I COMMONLY OBSERVE IN CLINICAL PRACTICE–
While trigeminal neuralgia is primarily a nerve condition, in clinical practice I often observe certain physical and behavioural patterns developing over time.
Common observations include:
- Increased neck and upper cervical stiffness
- Forward head posture, especially during prolonged sitting or phone use
- Tight jaw, facial, and upper shoulder muscles
- Shallow breathing and increased tension during pain anticipation
- Heightened anxiety or fear of triggering pain
Many patients unknowingly hold their head, neck, and jaw very stiffly in an attempt to protect themselves from pain. While this response is natural, prolonged tension can further irritate the nervous system and contribute to more frequent or intense episodes. This is why, alongside medical management, gentle physiotherapy focusing on posture, muscle relaxation, breathing, and nervous system calming often plays a supportive role in improving comfort and daily function.
PHYSIOTHERAPY SUPPORT IN TRIGEMINAL NEURALGIA-
STEP 3- GENTLE TECHNIQUES TO IMPROVE DAILY COMFORT
Short note (very important):
Physiotherapy in trigeminal neuralgia is supportive and gentle. The focus is not on directly treating the nerve pathology, but on reducing tension, improving posture, calming the nervous system, and helping patients feel safer and more comfortable in daily life. All techniques should remain within comfort and be performed under guidance when needed.
The aim is not to provoke symptoms, but to reduce overall tension in the neck, jaw, and nervous system. Many patients find these techniques helpful when practiced calmly and consistently.
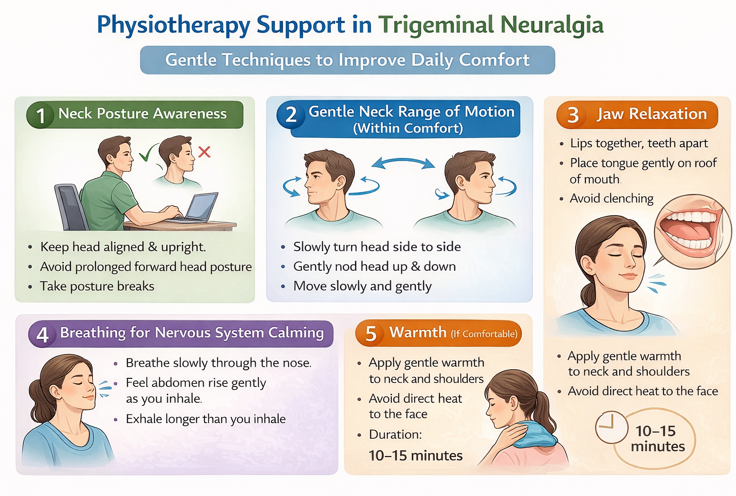
1.Neck Posture Awareness
Poor neck posture can increase tension around the upper cervical region and sensitise the nervous system.
What to do:
- Keep the head aligned over the shoulders
- Avoid prolonged forward head posture
- Take short posture breaks every 30–40 minutes
Clinical note:
This is posture awareness, not forced correction
2. Gentle Neck Range of Motion (Within Comfort)
What to do:
- Slowly turn the head right and left within pain-free range
- Gently nod the head up and down
- Keep movements slow and relaxed
How often:
1–2 times a day, 4–5 repetitions each
Stop if:
Facial pain is triggered.
3.Jaw Relaxation
Many patients hold their jaw tightly without realising it.
What to do:
- Keep teeth slightly apart at rest
- Place the tongue gently on the roof of the mouth
- Avoid clenching during stress
Simple cue:
“Lips together, teeth apart.”
4.Breathing for Nervous System Calming
Shallow breathing increases nervous system sensitivity.
What to do:
- Breathe slowly through the nose
- Allow the abdomen to rise gently
- Exhale longer than you inhale
- Duration:
3–5 minutes, 1–2 times a day
Warmth (If Comfortable)
How to use:
- Apply gentle warmth to the neck or shoulder region
- Avoid direct heat on the face unless advised
Duration:
10–15 minutes
Important Safety Notes
- Techniques should never increase facial pain
- Avoid aggressive stretching, massage, or self-treatment
- Stop if symptoms worsen and consult a professional
- Physiotherapy supports comfort; it does not replace medical care
STEP 4- HOME CARE & LIFESTYLE SUPPORT
Daily Habits That Help Reduce Flare-Ups
This section focuses on simple, gentle daily habits that support the nervous system and help reduce unnecessary triggers. These are supportive measures, not strict rules.
1.Protecting the Face from Cold & Sudden Stimuli-
Cold air and sudden temperature changes can trigger facial pain in some patients.
Helpful tips:
- Cover the face gently in cold or windy weather
- Avoid direct exposure to air conditioners or fans on the face
- Use lukewarm water for washing the face
Small temperature adjustments can make a noticeable difference.
2.Sleep Position & Neck Support
Poor neck support during sleep can increase tension around the upper cervical region.
What helps:
- Use a pillow that supports the natural curve of the neck
- Avoid very high or very flat pillows
- Side or back sleeping is usually better tolerated than stomach sleeping
Comfort matters more than perfect posture.
3.Managing Stress & Mental Tension
Stress does not cause trigeminal neuralgia, but it can increase pain intensity and frequency.
Helpful strategies:
- Short relaxation or breathing breaks during the day
- Gentle walking or stretching
- Calming routines before sleep
4.OM Mantra Chanting – For Neck Relaxation & Calm)
In clinical practice, some patients find that slow chanting of “OM” helps relax the neck, jaw, and shoulder muscles and brings calm to the nervous system.
From a physiological point of view, slow chanting:
- Encourages prolonged exhalation
- Reduces neck and jaw muscle tension
- Activates the body’s calming (parasympathetic) response
How to practice:
- Sit or lie comfortably with the neck supported
- Gently close the eyes
- Inhale slowly through the nose
- Exhale while softly chanting “OM”
- Keep the sound gentle and relaxed
Duration:
🕒 3–5 minutes, once or twice daily
Important note:
This practice is optional. Any calming activity that relaxes the neck and breathing can be used instead.
5.Eating & Oral Care (Without Fear)
Chewing and brushing can feel stressful during flare-ups.
Helpful tips:
- Prefer softer foods during pain episodes
- Avoid very hot, cold, or hard foods when pain is active
- Use a soft-bristled toothbrush
- Brush slowly and gently
The aim is comfort, not avoidance.
6.Staying Active — Without Overdoing It
Complete rest can increase stiffness and sensitivity.
What helps:
- Gentle daily movement
- Short walks within comfort
- Avoiding long periods of immobility
Movement should feel safe and calming, not forced.
🌿 Key Reassurance for Patients
Managing trigeminal neuralgia is about reducing triggers, not restricting life. With supportive daily habits, many patients find flare-ups become less frequent and easier to manage
STEP 5- DIET, SUPPLEMENTS & SUPPORTIVE REMEDIES
A Gentle, Supportive Approach for Nerve Health
Trigeminal neuralgia is a neurological condition and must be managed under medical supervision. The practices mentioned below are supporStive measures that I use cautiously in suitable patients to help calm the nervous system, support nerve health, and improve overall well-being. These do not replace medical treatment and may not be appropriate for everyone.
- Nasya Oil Therapy (Supportive Care)
Role of Nasya Oil Therapy in Nervous System Support
Why Nasya Matters in Facial Nerve Sensitivity?
Over the years in clinical practice, I have noticed that patients with facial nerve sensitivity often respond well when we calm the sensory system first — and Nasya oil therapy is one of the most reliable ways I have seen to do this.
From a nervous system perspective, the nasal cavity provides a sensory pathway linked to the trigeminal nerve and autonomic nervous system. Gentle nasal oil application helps maintain mucosal moisture and may reduce local irritation and nerve hypersensitivity. The sensory calming effect of Nasya is thought to support parasympathetic activation, helping shift the nervous system out of a persistent “fight-or-flight” state. In trigeminal neuralgia, this may reduce excessive nerve reactivity and improve tolerance to daily triggers.
Used consistently and correctly, Nasya can support sensory regulation and facial comfort. Thus, it may help create a calmer, more stable environment for the nervous system to respond better to other treatments.
How to perform Nasya:
- Best time: Morning (empty stomach) or early evening in a calm environment
- Lie comfortably with the neck gently extended backward (below 90°)
- Warm the oil slightly (lukewarm, not hot)
- Put 3–4 drops of oil into each nostril
- Inhale gently without force
- Remain relaxed for 1–2 minutes, then spit out any oil that reaches the throat
Frequency:
🕒 Up to 3 times daily, if well tolerated
Oils commonly used:
- Anu Taila
- Plain sesame oil (if advised)
- Other medicated nasal oils as recommended
Practical tips:
- Perform in a warm, calm setting
- Avoid immediately after meals
- Do not sniff forcefully
- Stop if irritation occurs
Consistency and gentleness are more important than quantity.

2.Brahmi (Bacopa Monnieri)
Support for the Nervous System & Mental Calm
Brahmi is an Ayurvedic herb traditionally used to support brain function, nerve health, and mental balance. In trigeminal neuralgia, it is mainly used to calm the nervous system rather than directly relieve pain.
It may help reduce nerve sensitivity, support relaxation and sleep quality, lower anxiety related to pain anticipation, and improve stress tolerance. This is especially relevant, as many patients experience mental exhaustion and constant alertness alongside pain.
How it is commonly taken?
Tablets, capsules, or powder, usually twice daily after meals, as per standard dosage or practitioner advice. Consistency matters more than high doses.
Clinical note: Effects are gradual and build over time.
3.Ashwagandha
Support for Stress Regulation, Sleep & Nervous System Balance
Ashwagandha is an adaptogenic herb traditionally used to help the body manage stress and support nervous system balance. In trigeminal neuralgia, it may be helpful when pain is associated with poor sleep, anxiety, fatigue, or constant mental tension.
It may reduce stress-related nervous system overactivity, support better sleep quality, and improve physical and mental resilience. Many patients find that when sleep and stress improve, pain episodes become easier to tolerate.
How it is commonly taken?
Powder or capsules, often taken at bedtime. Common practice includes about 5 g daily or 1 teaspoon of powder mixed in warm water, as per practitioner guidance.
Clinical notes: Benefits are gradual. It works best when combined with breathing practices, relaxation, and gentle physiotherapy. Some individuals may experience heaviness or drowsiness, in which case dose adjustment may be needed.
4.Lion’s mane (hericium erinaceus)
Support for Nerve Health & Repair Pathways
Lion’s Mane is a medicinal mushroom that has gained attention for its potential role in supporting nerve health and regeneration pathways. In trigeminal neuralgia, it is sometimes used as a supportive supplement alongside medical and physiotherapy care.
Why Lion’s Mane Is Considered?
Based on available research and clinical use, Lion’s Mane may help by:
- Supporting nerve growth factors involved in nerve repair
- Reducing low-grade neuro-inflammation
- Supporting cognitive clarity and mental resilience
- Helping patients feel more stable during long-term recovery
It is not a painkiller and does not act immediately. Its role is more supportive and long-term.
How It Is Commonly Taken?
- Form: Capsule or powder
- Timing: Usually once or twice daily, often after meals
- Dosage:1gm or as per product recommendation or practitioner guidance
Consistency over weeks matters more than short-term use.
Practical Clinical Notes
- Benefits, if any, are slow and gradual
- Works best when combined with stress regulation, adequate sleep, and physiotherapy
5.Omega-3 Fatty Acids
In my clinical experience, Omega-3s often make other supportive strategies work more effectively — especially when patients combine them with steady lifestyle changes and gentle physiotherapy.
Omega-3s (EPA + DHA) provide anti-inflammatory and neuroprotective support, helping calm irritated facial nerves and improving tolerance to everyday triggers. Consistent use can reduce neuro-inflammation and support nerve membrane stability, creating a more receptive environment for other treatments.
Sources: salmon, sardines, walnuts, flaxseed; supplements (fish oil / algae oil)
Supportive dose: 1000–2000 mg/day EPA+DHA (individual needs vary)
Caution: blood thinners, bleeding disorders, pre-surgery — use under guidance
6.Nerve pain support formulations-
In some patients, combination nerve-support supplements are used to help reduce nerve-related discomfort and low-grade inflammation. These formulations are not painkillers, but may support nerve nutrition and improve comfort, making it easier for patients to stay active and follow physiotherapy and lifestyle measures. They are usually taken once or twice daily after meals for a limited period and reviewed based on individual response. Their role is supportive and works best when combined with medical care, stress management, and gentle movement.
7.B-Vitamins (Supportive Supplement)
I often find that patients feel more stable and less reactive when their B-vitamin status is supported — especially B1, B6, and B12.
B-vitamins help maintain healthy nerve signaling and energy metabolism, and may reduce sensory hypersensitivity when levels are low. In trigeminal neuralgia, they can offer baseline support for nerve repair and resilience, making it easier for the nervous system to respond to other treatments.
Key forms:
- B1 (Thiamine / Benfotiamine): supports nerve pain sensitivity
- B6 (Pyridoxine / P-5-P): supports neurotransmitter balance
- B12 (Methylcobalamin): supports myelin health & nerve repair
Supportive dose ranges: (general guidance — varies by individual needs)
- B1: 50–300 mg/day
- B6: 10–50 mg/day (do not exceed long-term without guidance)
- B12: 1000–2000 mcg/day (or as advised)
Caution: very high B6 intake over time may worsen nerve symptoms — stay within guided ranges.
8.Magnesium (supportive):
Magnesium plays an important role in calming overactive nerves and supporting healthy nerve signaling. For some people, it can help ease nerve irritability, reduce associated muscle tension, and improve sleep quality—factors that often influence how strongly pain is felt. While it does not cure trigeminal neuralgia, magnesium may provide meaningful supportive relief when used alongside medical treatment under professional guidance.
9.Oil pulling (morning routine – supportive care)
Oil pulling with coconut oil is traditionally used to support oral hygiene and relaxation of the jaw and facial muscles. In patients with trigeminal neuralgia, it may help reduce jaw tension and morning stiffness when done gently. Typically, 1 tablespoon of coconut oil is swished softly in the mouth for 5–10 minutes in the morning, then spat out. Vigorous swishing should be avoided; the focus is relaxation, not force.
10.Ghee application at the navel (vata support – night routine)
In traditional Ayurvedic practice, applying a small amount of warm ghee at the navel (nabhi) is believed to support grounding and balance dryness associated with Vata imbalance, which is often linked with nerve sensitivity. Some patients find this calming and helpful for sleep. It is usually done at bedtime, using a few drops of warm ghee, applied gently over the navel and left overnight. This is a comfort-based, optional practice.
11.Pranayama & hydration (daily nervous system support)
Gentle pranayama helps regulate the nervous system and reduce pain sensitivity by calming excessive sympathetic activity. Slow, comfortable breathing practices can be done for 10–15 minutes daily, preferably in a quiet, relaxed setting. Alongside this, adequate hydration throughout the day supports nerve conduction, muscle function, and overall recovery. Small, regular sips of water are preferable to large amounts at once.
STEP 6- DIET FOR NERVE HEALING & NERVOUS SYSTEM CALM
Supportive Nutrition for Trigeminal Neuralgia
Diet does not cure trigeminal neuralgia, but the right food choices can support nerve health, reduce inflammation, and stabilise the nervous system. The goal is nourishment and balance, not restriction.
Foods that support nerve health-
What to Focus On | Examples | Why It Helps |
Healthy Fats (very important) | Ghee (small), coconut oil, olive oil, walnuts, almonds, flaxseeds, chia | Supports nerve insulation, reduces dryness linked to nerve sensitivity |
Protein for Nerve Repair | Lentils/dals, beans, tofu, tempeh, eggs, paneer, curd (if tolerated) | Helps nerve repair, muscle relaxation, recovery |
B-Vitamin Foods | Whole grains (millets, oats, brown rice), leafy greens, bananas, fermented foods, nuts | Essential for nerve function & resilience; supports recovery |
Anti-Inflammatory Fruits & Veggies | Greens, pumpkin, carrots, sweet potato, berries, amla, apples, broccoli | Reduces inflammation, supports nervous system stability |
Warm & Grounding Eating Pattern | Warm cooked meals, regular timings, small balanced portions | Improves tolerance; gentler on sensitive nerves |
Foods & Habits to Limit During Flare-Ups
May Worsen Sensitivity | Reason / Note |
Very cold foods/drinks | Temperature sensitivity may trigger flares |
Excess caffeine | Can increase nervous system reactivity |
Processed & packaged foods | Higher inflammatory load |
Excess refined sugar | May increase inflammatory responses & fatigue |
Skipping meals, long fasting | Can destabilise energy & nerve sensitivity |
Warm, grounding foods are generally better tolerated than dry or cold foods.
🌿 A Gentle Healing Note
Pain can make the nervous system stay in a constant state of alert. Along with medical care, calming the mind and body plays an important role in recovery.
Many patients find it helpful to pause daily and remind themselves:
“My nervous system is safe.
My body is learning to calm itself.
With proper care, support, and patience, I am moving toward comfort and balance.”
This is not about denying pain — it is about reducing fear, which often amplifies nerve sensitivity. A calm mind supports better healing responses, improved sleep, and more confident participation in treatment.
🌿 Simple Clinical Reminder
Diet supports nerve healing slowly and steadily. When combined with medical care, physiotherapy, breathing practices, and good sleep, it helps create a calmer internal environment for recovery.
A Final Reassuring Note
Trigeminal neuralgia can be distressing, especially when pain appears suddenly. With proper medical care, gentle physiotherapy support, and calming daily practices, many patients learn to manage symptoms better over time. Improvement is usually gradual, but even small gains in comfort and confidence are meaningful.
This article shares the same calm, practical guidance I offer my patients in the clinic — focused on understanding, support, and steady care rather than fear or false promises.
Need Personalized Guidance?
If you feel unsure about your symptoms or need individualized guidance beyond general information, you may consider a personal consultation.
Affiliate & Medical Disclaimer
Some links in this article are affiliate links, meaning I may earn a small commission at no extra cost to you. This support allows me to continue creating free, evidence-based health guides, exercises, and educational content. All recommendations are shared based on clinical experience and general wellness principles and are not intended to diagnose or treat medical conditions. Please consult a qualified healthcare professional before starting any supplement or treatment.
About Me
Chaya Gray
Quis autem vel eum iure repreherit qui in ea voluptate velit ess quam nihil molestiae consequatur velab illum denounci pleasure
Recent Blogs

Conveniently deploy accurate …

Conveniently deploy accurate …