Posted By
Chaya Gray
Date
March 31, 2025
Comments
0
Sciatica: Relieving Nerve Pain from the Back to the Leg
Introduction
Many people live with sciatica for months or even years, trying painkillers, rest, or random exercises, yet the pain keeps returning. In my clinical experience, one of the most common reasons is that sciatica is often treated only at the site of pain, not at its source.
Sciatica pain can be confusing. Some people feel intense leg pain with very little back discomfort, while others are unsure whether the problem is in the spine, hip, or muscles. This uncertainty often leads to fear, delayed treatment, or ineffective self-management.
This article is freely shared to help you understand sciatica in a clear, practical way, exactly how it is explained during physiotherapy consultations. You will learn:
- What sciatica actually is (and what it is not)
- Why the pain travels from the back to the leg
- How physiotherapists assess sciatica clinically
- Which exercises and posture corrections truly help
- When sciatica improves with conservative care and when further evaluation is needed
The goal of this guide is not just pain relief, but helping you understand how to manage sciatica safely and confidently, using a structured physiotherapy-based approach.
Many people live with sciatica for months or even years, trying painkillers, rest, or random exercises, yet the pain keeps returning. In my clinical experience, one of the most common reasons is that sciatica is often treated only at the site of pain, not at its source.
Sciatica pain can be confusing. Some people feel intense leg pain with very little back discomfort, while others are unsure whether the problem is in the spine, hip, or muscles. This uncertainty often leads to fear, delayed treatment, or ineffective self-management.
This article is freely shared to help you understand sciatica in a clear, practical way, exactly how it is explained during physiotherapy consultations. You will learn:
- What sciatica actually is (and what it is not)
- Why the pain travels from the back to the leg
- How physiotherapists assess sciatica clinically
- Which exercises and posture corrections truly help
- When sciatica improves with conservative care and when further evaluation is needed
The goal of this guide is not just pain relief, but helping you understand how to manage sciatica safely and confidently, using a structured physiotherapy-based approach.
Step 1 – Understanding Sciatica
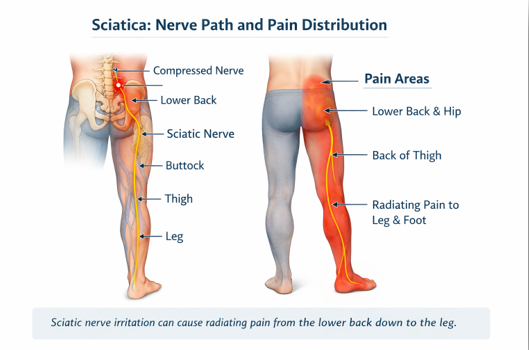
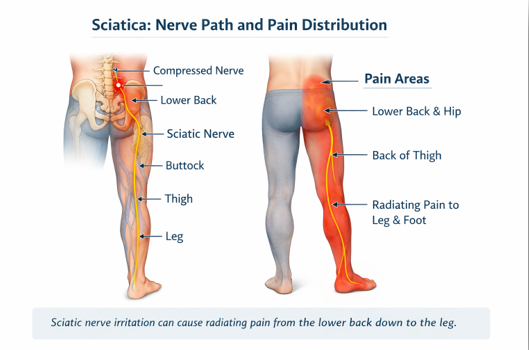
Sciatica is not a disease by itself; it is a pattern of nerve-related pain. It occurs when the sciatic nerve, the longest nerve in the body, becomes irritated or compressed.
The sciatic nerve:
- Originates from the lower spine (lumbar region)
- Passes through the buttock
- Travels down the back of the thigh
- Extends into the leg and foot
When this nerve is affected, pain is felt along its course rather than staying limited to the lower back. This explains why many people feel leg pain even when back pain is mild or absent.
In clinical practice, patients often focus only on leg pain. However, in most cases, the source of sciatica lies in the lower back or pelvic region. Understanding this connection is the first step toward effective treatment.
Step 2 – Why Sciatica Happens
Sciatica occurs when the sciatic nerve or its nerve roots are compressed, irritated, or stretched. The compression usually happens near the lower spine, even though pain is often felt in the leg.
Common Causes of Sciatica
- Disc bulge or disc herniation
A bulging or slipped disc in the lower spine can press on the nerve roots forming the sciatic nerve. - Prolonged sitting and poor posture
Long hours of sitting increase pressure on the lumbar spine and nerve structures, especially with slouched posture. - Muscle tightness
Tightness in the lower back, buttock muscles (including the piriformis), or hamstrings can irritate the sciatic nerve. - Improper lifting or sudden movements
Bending, twisting, or lifting without proper technique can strain spinal structures and trigger nerve irritation. - Reduced spinal mobility
Stiffness in the lumbar spine alters load distribution and increases stress on nerve tissues.
Because these factors often develop gradually, sciatica may begin as mild discomfort and worsen over time if the underlying cause is not addressed.
Step 3 – How Sciatica Feels (Symptoms & Pain Pattern)
Sciatica has a very characteristic pain pattern because it involves irritation of a nerve rather than only muscles or joints.
Common Symptoms
People with sciatica may experience:
- Pain that starts in the lower back or buttock and travels down the leg
- Sharp, shooting, burning, or electric-like pain
- Pain felt along the back of the thigh, calf, or into the foot
- Tingling, numbness, or a “pins and needles” sensation in the leg or foot
- Weakness or heaviness in the affected leg
The pain is often one-sided, affecting only one leg at a time.
Aggravating Factors
Sciatica pain commonly worsens with:
- Prolonged sitting
- Bending forward
- Lifting objects
- Sudden movements or twisting
- Sitting on low or soft surfaces
Some people notice relief while standing or walking, while others feel better lying down, depending on the cause.
How Sciatica Differs from Simple Back Pain
Unlike general low back pain:
- Sciatica pain radiates down the leg
- Leg pain may be more severe than back pain
- Movements that stretch or compress the nerve increase symptoms
Recognizing this pattern is important, because treatment focuses on reducing nerve irritation, not just relieving back discomfort.
Step 4 – Physiotherapy Assessment (What I Examine Clinically)
When a patient presents with sciatica, my assessment focuses on identifying where and why the sciatic nerve is being irritated.
I assess:
- History and onset of pain, including posture, activities, and aggravating movements
- Posture and movement patterns, especially during sitting, bending, and walking
- Lumbar spine mobility, noting pain or restriction with specific movements
- Neural tension, to check how the sciatic nerve responds to movement
- Muscle flexibility and strength, particularly in the lower back, hips, and legs
This assessment helps determine whether sciatica is driven by spinal compression, muscle-related nerve irritation, or movement dysfunction, allowing treatment to be targeted and effective.
Step 5 – Physiotherapy Exercises for Sciatica
These exercises aim to reduce nerve irritation, improve mobility, and support recovery. They should be performed gently and within a pain-free range.
1. Pelvic Tilt Exercise
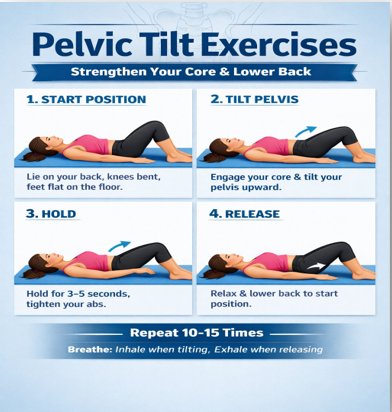
How to do it:
- Lie on your back with knees bent
- Gently tighten your abdominal muscles
- Flatten your lower back into the bed
- Hold for 5 seconds, then relax
Repetitions:
8–10 times, 2–3 times daily
Purpose:
Reduces lower back stiffness and improves spinal control.
2. Knee to Chest Exercise (Single Leg)
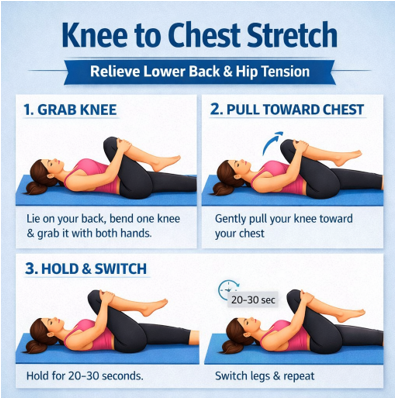
How to do it:
- Lie on your back
- Slowly bring one knee toward your chest
- Hold with both hands for 10 seconds
- Return to starting position
Repetitions:
5–8 times on each side
Purpose:
Improves lumbar mobility and reduces nerve pressure.
3.Sciatic Nerve Glide (Gentle)
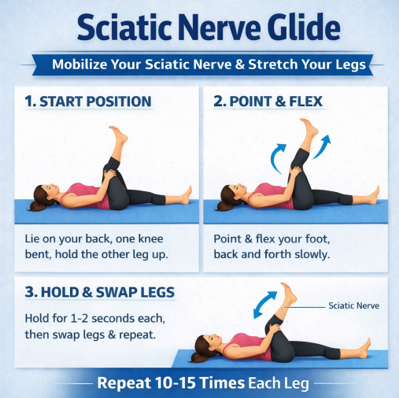
How to do it:
- Lie on your back
- Lift one leg with knee slightly bent
- Slowly straighten the knee while pulling toes toward you
- Bend the knee again and relax
Repetitions:
5–6 gentle repetitions
Purpose:
Improves movement of the sciatic nerve without overstretching.
4. Hamstring Stretch
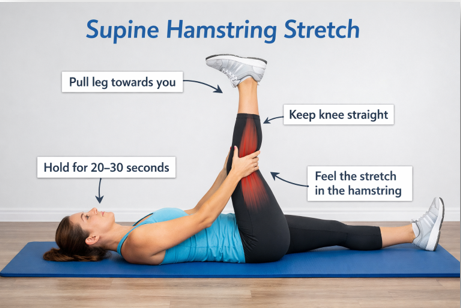
How to do it:
- Lie on your back
- Raise one leg and hold behind the thigh
- Gently straighten the knee until a stretch is felt
- Hold for 15 seconds
Repetitions:
3 repetitions on each side
Purpose:
Reduces tension on the sciatic nerve.
5. Glute Stretch (Figure-4 Stretch)

How to do it:
- Lie on your back
- Place one ankle over the opposite knee
- Gently pull the supporting thigh toward your chest
- Hold for 15 seconds
Repetitions:
3 repetitions on each side
Purpose:
Relieves buttock muscle tightness that can irritate the nerve.
⚠️ Exercise Precautions
- Stop if leg pain increases significantly
- Avoid forceful stretching
- Progress exercises only after pain reduces
Step 5B – Exercise Progression (When Pain Has Reduced)
Once leg pain and nerve sensitivity have reduced, additional exercises are introduced to strengthen the spine, improve stability, and prevent recurrence. These exercises should be started only when basic movements are comfortable.
6.Bridge Exercise

How to do it:
- Lie on your back with knees bent
- Tighten your abdominal muscles
- Lift your hips slowly off the bed
- Hold for 5 seconds, then lower
Repetitions:
8–10 repetitions
Purpose:
Strengthens gluteal and lower back muscles, improving spinal support.
7. Quadruped Arm–Leg Raise (Bird Dog)

How to do it:
- position your self on hand and knees
- Extend one arm and the opposite leg
- keep your spine netural
- hold for 5 seconds , then switch sides
Repetitions:
6–8 repetitions
Purpose:
Improve core stability and spinal control
8.Standing Back Extension (Pain-Free Range)
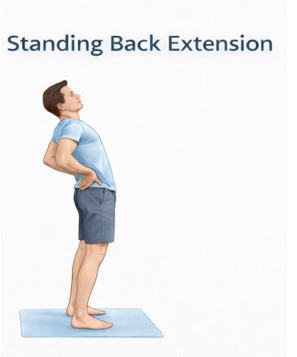
How to do it:
- Stand upright with hands on hips
- Gently bend backward within comfort
- Return to neutral
Repetitions:
6–8 repetitions
Purpose:
Helps restore lumbar extension mobility in selected individuals.
9. Side-Lying Clamshell

How to do it:
- Lie on your side with knees bent
- Keep feet together and lift the top knee
- Do not rotate the pelvis
Repetitions:
10 repetitions on each side
Purpose:
Strengthens hip stabilizers, reducing strain on the lower back.
⚠️ Progression Guidelines
- Start only after leg pain reduces
- Exercises should not reproduce radiating pain
- Progress gradually under physiotherapist guidance
Step 6 – Home Care & Daily Activity Advice for Sciatica
Simple daily habits can significantly support recovery from sciatica.
- Sitting: Keep the lower back supported, feet flat, and avoid slouching. Take breaks every 30–40 minutes.
- Sleeping: Sleep on the side with a pillow between the knees or on the back with a pillow under the knees. Avoid stomach sleeping.
- Bending & lifting: Bend at the hips and knees, avoid twisting, and keep objects close to the body.
- Activity: Avoid prolonged bed rest. Gentle walking is usually helpful.
These measures reduce spinal strain and help calm nerve irritation.
Step 7 – Diet, Supplements & Supportive Care for Sciatica
In my clinical experience, while physiotherapy remains the foundation of sciatica treatment, diet and supportive supplements play a very important role in recovery, especially in patients with prolonged pain, nerve sensitivity, or frequent flare-ups. Many patients notice better pain control, improved tolerance to exercises, and faster recovery when these aspects are addressed properly.
Dietary changes and supplements can be helpful for many people with sciatica. However, individual needs may vary, so it is always advisable to discuss supplements with your doctor –especially if you have other medical conditions or are on long-term medications.
Why Diet & Supplements Matter in Sciatica
Sciatica involves nerve irritation, muscle guarding, and fatigue. Supporting the body with the right nutrients helps:
- Calm irritated nerves
- Reduce muscle tightness and fatigue
- Improve tissue healing and recovery
- Enhance the effectiveness of physiotherapy exercises
Dietary Support (What I Commonly Advise Patients)
A simple, balanced diet focused on nerve and muscle health can make a noticeable difference.
Helpful food choices include:
- Protein sources: eggs, milk, curd, yogurt, lentils, beans, chickpeas
- Magnesium-rich foods: nuts, seeds, green leafy vegetables, whole grains
- Anti-inflammatory foods: fruits, vegetables, turmeric, ginger
- Healthy fats: nuts, seeds, olive oil
Adequate hydration is equally important, as dehydration can increase muscle stiffness and discomfort.
💊 STEP 8- Supplements (A Supportive Boost When Needed)
When used appropriately, supplements can meaningfully support physiotherapy outcomes by enhancing muscle recovery, nerve health, and overall resilience. They work best when tailored to individual needs and combined with active rehabilitation.
- Magnesium – Helps ease muscle tightness, reduce cramps, and supports healthy nerve signaling, making movement and exercise more comfortable.
- Vitamin B12 – Plays a key role in nerve repair and energy production, particularly beneficial for individuals with nerve-related pain, tingling, or persistent fatigue.
- Vitamin D – Essential for bone strength, muscle function, and immune health; supplementation can improve recovery when levels are insufficient.
- Curcumin – A natural anti-inflammatory compound that may aid in pain modulation and support tissue healing during rehabilitation.
- Ashwagandha – Known for its adaptogenic properties, it may help manage stress-related muscle tension, improve endurance, and support overall physical recovery.
Supplements are intended to complement physiotherapy—not replace exercise, movement retraining, or lifestyle modification.
Some patients also find relief with nerve-support formulations-
such as Nerve Pain Relief products (e.g., Miduty brand), used as an adjunct, not a replacement for treatment.
Supplements are best chosen based on individual needs and response, and they work most effectively when combined with physiotherapy and posture correction.
Supportive Measures
- Heat therapy to the lower back or buttock for 10–15 minutes can help relax muscles
- Adequate rest, sleep, and stress management further support nerve recovery
🟢 Clinical Takeaway
Physiotherapy addresses the mechanical cause of sciatica, while diet and supplements help support nerve healing and muscle recovery. When used together, many patients experience better symptom control and smoother rehabilitation.
Step 8 – Do’s & Don’ts in Sciatica
✅ Do’s
- Maintain good posture while sitting and standing
- Take regular breaks from prolonged sitting
- Continue gentle walking and daily activities as tolerated
- Perform prescribed physiotherapy exercises regularly
- Use heat therapy if it provides relief
- Sleep in a spine-supported position (side or back)
❌ Don’ts
- Avoid prolonged bed rest
- Do not sit for long hours without breaks
- Avoid sudden bending, twisting, or heavy lifting
- Do not perform forceful stretching during active pain
- Avoid ignoring worsening leg pain, numbness, or weakness
- Do not self-progress exercises aggressively without guidance
Following these do’s and don’ts helps prevent flare-ups, supports nerve healing, and improves long-term outcomes in sciatica.
Step 9 – Red Flags (When to Seek Medical Attention)
Most cases of sciatica improve with conservative care such as physiotherapy, exercises, and lifestyle modification. However, certain symptoms require urgent medical evaluation.
Seek medical attention if you experience:
- Progressive weakness in the leg or foot
- Severe or worsening numbness in the leg
- Loss of bladder or bowel control
- Numbness in the groin or saddle area
- Severe pain that does not improve despite rest and treatment
- Sciatica following a significant fall or injury
- Pain associated with unexplained weight loss, fever, or night pain
These symptoms may indicate serious nerve compression or underlying conditions that need prompt medical care.
Clinical Note
Early recognition of red flags ensures timely intervention and helps prevent long-term nerve damage.
Conclusion
Sciatica can be painful and disruptive, but in most cases, it is manageable and reversible with the right approach. Understanding that sciatica is a nerve-related condition—often originating from the lower back—helps guide effective treatment rather than just temporary pain relief.
Physiotherapy plays a central role by:
- Reducing nerve irritation
- Restoring movement and strength
- Correcting posture and daily habits
- Preventing recurrence
When exercises, home care, and lifestyle advice are combined with supportive measures such as proper nutrition and selected supplements, many patients experience significant and lasting improvement. Early assessment and consistent care are key to successful recovery.
Frequently Asked Questions (FAQs)
- Is sciatica permanent?
No. Most cases of sciatica improve with physiotherapy, exercises, and proper activity modification. Persistent symptoms usually indicate an untreated underlying cause.
- Is walking good for sciatica?
Gentle walking is often beneficial and helps reduce stiffness. However, it should be done within a comfortable range and avoided if it significantly worsens pain.
- Can exercises worsen sciatica?
Exercises performed incorrectly or progressed too early can aggravate symptoms. This is why exercises should be pain-free and gradually progressed under guidance.
- Does sciatica require surgery?
Most people with sciatica do not need surgery. Conservative treatment is effective in most cases. Surgery is considered only when severe or progressive neurological symptoms are present.
- How long does recovery usually take?
Some people improve within a few weeks, while others may take longer depending on the cause and severity. Consistency with treatment plays an important role.
Need Personalized Guidance?
If you are experiencing ongoing symptoms related to this condition or feel unsure about your recovery, a personalized physiotherapy assessment can help identify the exact cause and guide appropriate treatment. You may book a one-to-one consultation for condition-specific evaluation and care.
Medical & Affiliate Disclosure
Some links in this article are affiliate links, meaning I may earn a small commission at no extra cost to you. This support allows me to continue creating free, evidence-based health guides, exercises, and educational content. All recommendations are shared based on clinical experience and general wellness principles and are not intended to diagnose or treat medical conditions. Please consult a qualified healthcare professional before starting any supplement or treatment.
About Me
Chaya Gray
Quis autem vel eum iure repreherit qui in ea voluptate velit ess quam nihil molestiae consequatur velab illum denounci pleasure
Recent Blogs

Conveniently deploy accurate …

Conveniently deploy accurate …